
| | | We shall look first at normal development of the heart, and then at some of the more common heart defects. This will be followed by an overview of the development of the main blood vessels | 
| Normal development of the heart On completion of this section, you should be able to:  | give the timing of the main stages in heart development |  | describe the process of septation of the heart tube |  | explain development of the pericardial cavity and sac |
| 
| The need for a transport system During the pre-implantation period the conceptus is small and receives all the nutrients and gases it requires by simple diffusion from the surrounding fluid. Any waste products it generates diffuse out in the opposite direction. During implantation, the conceptus seems to derive some nutrition by breaking down the endometrial cells in its path and absorbing the breakdown products. When implantation is complete, the outer layer of the trophoblast - the syncytiotrophoblast - is in close relationship with maternal tissues and, more especially, maternal blood. From this time on, up until birth, the embryo and fetus will obtain its requirements from the maternal blood, and dispose of waste products into the maternal blood. This exchange between the fetal blood stream and the maternal blood stream occurs at the placenta. After the second week of development, the embryo has grown too large for all regions to receive what they require by simple diffusion through the trophoblast. During the third week, the circulatory system - the embryonic heart and blood vessels - begins to develop, and during the 4th week the heart begins to beat and pump blood through the system. The heart is the first embryonic organ to become functional, and it must continue to beat effectively, even though its own development is far from complete at this stage. First, look at the diagram below to appreciate the time scale of heart development. There is no need at this stage to memorize the exact timings of embryological events - these can always be looked up if needed. It is usually sufficient to remember that the period of intense morphogenesis for most organs and systems is the embryonic period, weeks 2 to 8. However, given that the heart is such an important part of the embryo, and given that abnormalities of the cardiovascular system are important from a practical point of view, it is well worth studying heart development with extra care. Another tip - focus most of your attention on the process of septation: the heart defects seen at birth most commonly stem from errors in this process. 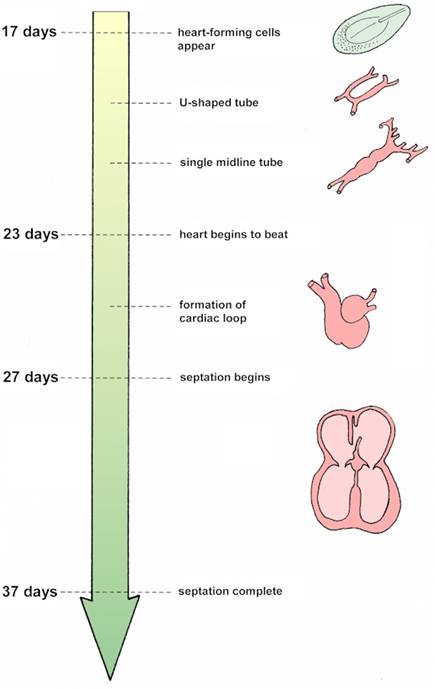
Development of the embryonic heart from 17 days
after conception to 37 days. Note how the single midline
tube becomes looped and then subdivided into 4 chambers. 
Pericardial cavity As you follow development of the heart, note how the pericardial cavity develops in relation to it. The pericardial cavity is formed from the most cranial part of the intra-embryonic coelom. You will see that the heart develops in splanchnic mesoderm with the cavity initially dorsal to it. Observe the changes in this relationship as the embryo folds. Try and work out why it is that the visceral pericardium has a different nerve supply from the parietal pericardium. 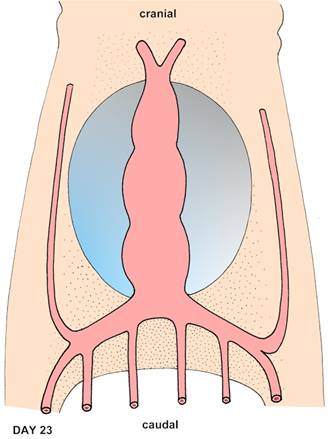
Heart tube - developing within the pericardial cavity (blue).
Note the veins converging on the caudal end of the heart
and the arteries leaving the cranial end. 
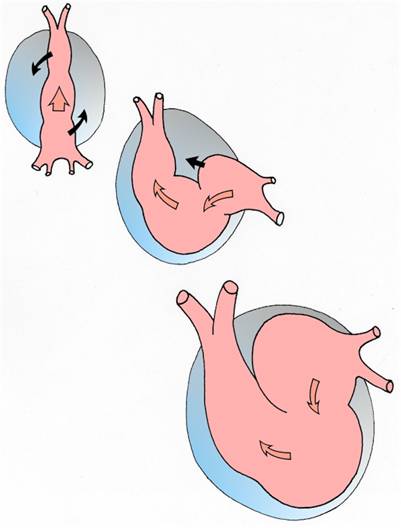
Formation of the cardiac loop - the developing atrium
is initially located caudally, but gradually moves cranially.
The next chamber, the ventricle, moves more caudally.
Blood leaving the ventricle enters the truncus arteriosus
before leaving the heart into the arterial system. 
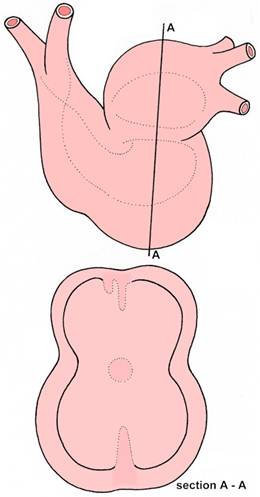
Septation dividing the chambers into left and right parts.
In section A - A, the septum primum and septum secundum
can be seen above within the atrium. These will grow down
to form the interatrial septum, forming the
foramen ovale as they do so.
The upward directed partition within the ventricle (below)
will form the muscular part of the interventricular septum.
The endocardial cushions more centrally
will contribute the membranous part
of the interventricular septum. 
| Questions on normal development of the heart How many days does it take the heart-forming cells to establish a 4-chambered heart? During which weeks of development does septation of the heart occur? What causes the midline heart tube to buckle and form the cardiac ‘loop'? What is the name given to the one-way valve in the pre-natal interatrial septum. What happens to this structure after birth? What portion of the heart receives returning venous blood? Describe the formation of the membranous part of the interventricular septum. What does the spiral septum subdivide? What structures are formed by this means? How is the pericardial sac formed?
| 
| Abnormal development of the heart When you have completed this section, you should be able to:  | list the more common abnormalities of the heart |  | give an embryological explanation for each of these abnormalities |  | deduce the possible consequences for the affected baby |
| 
| Septal defects Development of the heart can become abnormal at any stage. However, if a fault arises in one of its earliest stages of development, the consequences are severe and the embryo is likely to die, since it cannot survive without an efficient transport system. Abnormalities which arise later - particularly during the process of septation - are usually compatible with prenatal life, and are therefore more frequently encountered in newborn babies. Remember that birth defects of the cardiovascular system form a significant proportion of the clinical problems associated with the neonatal period. Although errors of septation may not be life-threatening before birth, their harmful effects tend to become much more pronounced after birth, and surgical intervention may be required. The examples that follow are predominantly septal defects (read about other types of heart abnormality such as ectopia cordis and dextrocardia in your textbooks). For each example, note the location of the abnormality (or abnormalities) in the heart, and then try to work out an embryological explanation of how the error(s) arose. Later, when you have learned more about the major blood vessels and the pattern of blood flow before and after birth, come back to these cardiac abnormalities again and try to work out what the consequences might be for the baby, before and after birth. 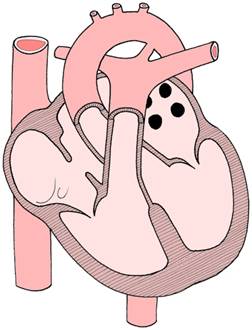
atrial septal defect - the foramen ovale
is patent rather than forming a one-way valve
between the right atrium and left atrium.
This will allow abnormal shunting of blood
between the atria after birth. 
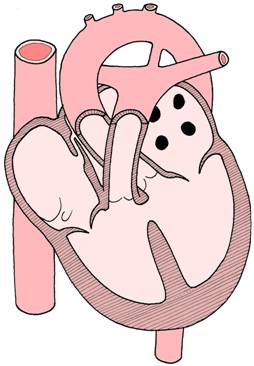
ventricular septal defect - the membranous part
of the interventricular septum has failed to form
and blood can move abnormally
between the left and right ventricles. 
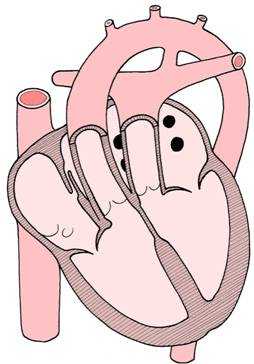 transposition of the great vessels - the aorta
exits from the right ventricle, and the pulmonary trunk
exits from the left ventricle.
This is only compatible with life postnatally
if the ductus arteriosus remains patent,
allowing communication between the otherwise closed
systemic and pulmonary circulations
driven by the left and right sides of the heart. 
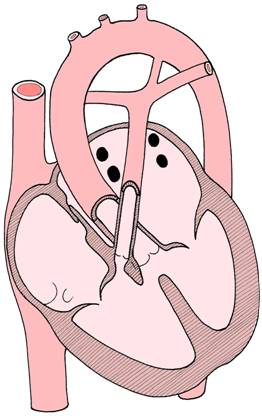
Tetralogy of Fallot - this syndrome of heart defects
is characterised by four features:
ventricular septal defect,
overriding aorta,
pulmonary stenosis,
and hypertrophy of the right ventricle. 
Questions on cardiac abnormalities What is probe patency of the foramen ovale? What is dextrocardia? What does cyanosis mean? In which part of the interventricular septum are defects most commonly found? What would be the effect of such an abnormality? What is meant by tricuspid atresia? What pattern of defects might you expect if the endocardial cushions fail to fuse? Can you name a viral infection that might cause cardiac defects if the mother is infected during the first trimester?
| 
| Development of the major arteries On finishing this section, you should be able to:  | describe the initially symmetrical arrangement of embryonic vessels |  | explain the changes that occur to produce the asymmetrical arrangement of arteries we see postnatally |  | give embryological explanations for the more common abnormalities of the major arteries, and suggest possible consequences |
| 
| Symmetrical start In the third week after conception, a network of blood vessels forms within the embryonic body, yolk sac, connecting stalk, and trophoblast. When the heart begins to beat on day 23, blood begins to move through this network. Soon, a symmetrical pattern of blood circulation is set up, with corresponding vessels on both sides of the embryo. Thus, there are:  | pairs of aortic arches around the pharyngeal part of the gut tube |  | paired dorsal aortae, supplying the embryonic body |  | paired vitelline arteries to the yolk sac |  | paired umbilical arteries to the trophoblast |  | paired cardinal veins draining the embryonic body |  | paired vitelline veins draining the yolk sac |  | paired umbilical veins returning from the trophoblast. |
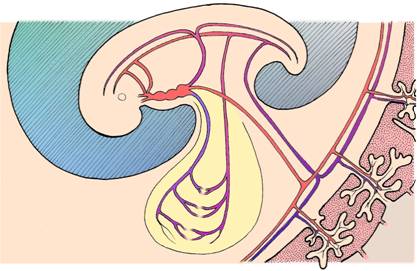
In this diagram, vessels are shown linking the embryo
with the yolk sac (yellow)
and the developing placenta (lower right).
Note the embryonic heart - identify the main blood vessels. 
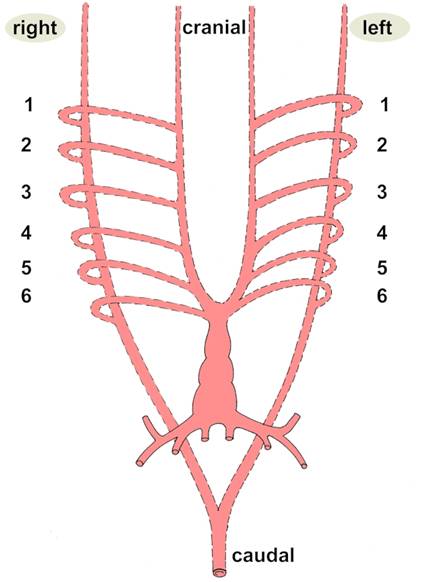
Symmetrical arrangement of major arteries -
this arrangement will become modified
when the heart undergoes changes in shape
and becomes divided into 4 chambers. 
Questions on development of arteries Which arteries supply the yolk sac? From which embryonic aortic arch is the definitive arch of the aorta derived? (‘Definitive' means the one we see finally when development is complete.) Describe development of the right subclavian artery. From what does the ductus arteriosus develop? What does it connect? What does it become after birth? What is meant by coarctation of the aorta? If this lesion is situated distal to the ductus arteriosus, what changes might you observe in the pattern of blood flow to the lower part of the body? Which structures may be constricted by a double aortic arch? Which aortic arches in the embryo are sometimes called the pulmonary arches?

Some examples of abnormal blood vessels 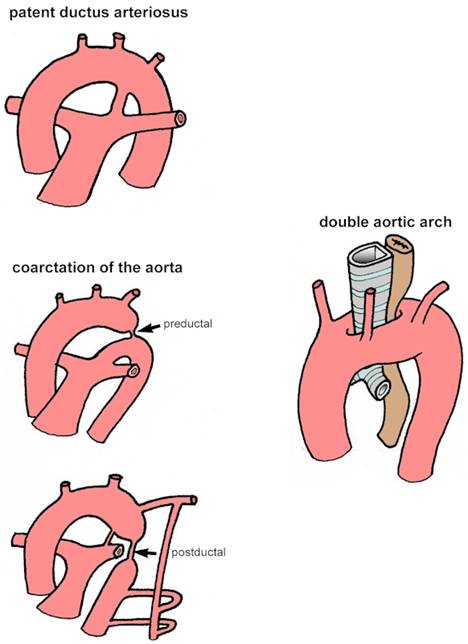
| 
| Development of the major veins On completing this section, you should be able to:  | describe in general terms the conversion of the initially symmetrical pattern of veins to the definitive, asymmetrical pattern |  | enumerate the more common types of major abnormalities of veins |  | describe the pattern of fetal circulation of blood, and the transition which occurs at birth to the postnatal pattern |
| 
| Variation in the venous system It is quite ‘normal' to find that veins show considerable variation - between sides of the same body and between people. These differences are usually of little clinical significance. The venous system operates at a lower pressure than the arterial system, and like the meandering course of a slow-moving river, veins sometimes follow irregular courses back to the heart. This is especially true of superficial veins. However, even with this variation, the basic pattern is usually recognisable. When studying the embryological development of the veins, do not become 'bogged down' with details. It is however helpful to note the general trend towards the right side: blood returning to the heart from the placental and systemic circulations is channelled in increasing quantities to the right horn of the sinus venosus. A major factor in this change is the development and rapid enlargement of the liver just caudal to the heart, where the great veins pass through the septum transversum. The only significant exception to this right-hand rule in seen in the retention of only one of the originally paired umbilical veins - it is the left umbilical vein which is retained! Note also the third circulatory shunt - the ductus venosus - which links the umbilical vein to the inferior vena cava, by-passing the liver sinusoids and facilitating blood return to the right atrium. (The other shunts are the foramen ovale and the ductus arteriosus.) The pulmonary veins are derived from an outgrowth from the atrium of the initial heart tube. This outgrowth branches in relation to the developing lung buds. 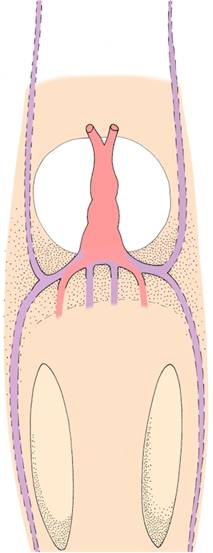 Symmetrical veins - note the pairs of veins
entering the sinus venosus.
The cardinal veins return blood from the embryonic body,
the vitelline veins from the yolk sac,
and the umbillical veins (pink)
return oxygenated blood from the placenta. 
Examples of abnormal veins 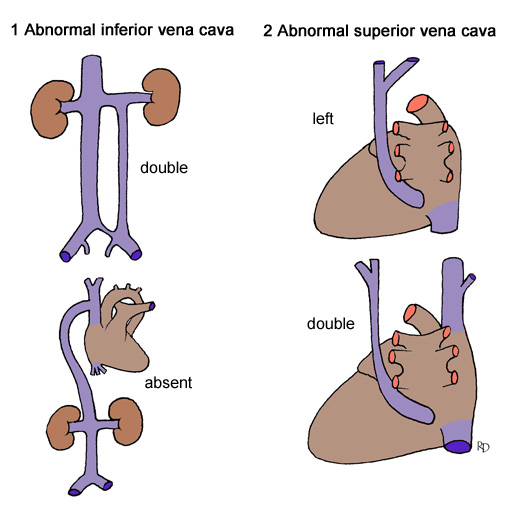
Abnormal arrangements of veins 
Questions on the development of the venous system What becomes of the left horn of the sinus venosus? How is the inferior vena cava formed? What effect does development of the liver have on veins passing through the septum transversum? Describe the ductus venosus. Does it carry oxygenated blood or deoxygenated blood? Which vessels pass through the fetal umbilical cord? Do the vitelline veins contribute to the formation of any important veins in the body? Into which structure would an abnormal left superior vena cava drain?

Circulatory changes at birth At birth, the baby begins to breath, the placental circulation closes down, and the three prenatal ‘shunts' are obliterated. 1 breathing begins - replacement of fluid in lungs with air 2 cessation of placental circulation, closure of ductus venosus 3 closure of foramen ovale 4 spasm and closure of ductus arteriosus
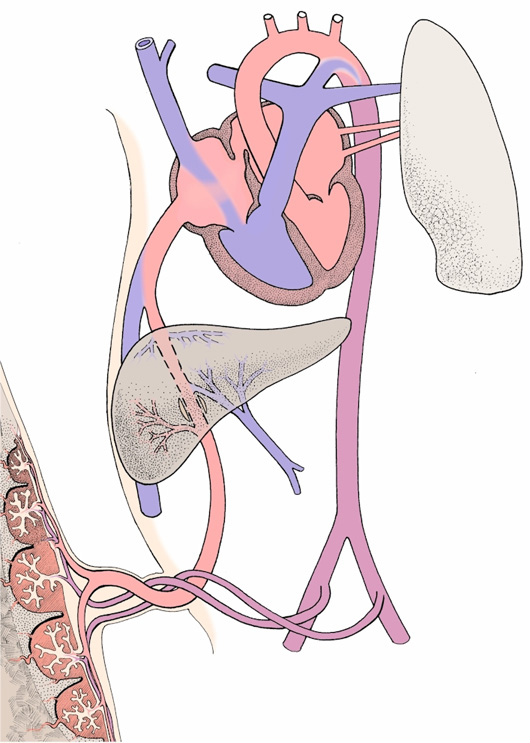
Pattern of prenatal circulation 
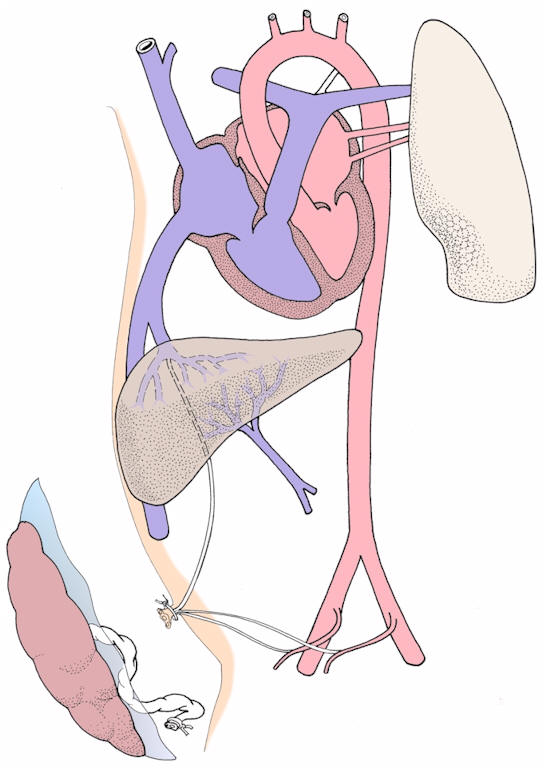
Pattern of postnatal circulation 
Questions on the fetal circulation and the transition at birth Why is it best to wait for a few minutes after the baby is delivered before tying and cutting the umbilical cord? What is the function of the foramen ovale before birth? In the adult heart, where is the fossa ovalis situated? What is thought to initiate closure of the ductus arteriosus? What causes a lowering of pulmonary resistance to blood flow after birth?
| 
|
|